MHQP and MSCA Seek New Research Directions for Sickle Cell Disease Pain Crisis Care
(April 2024)
 MHQP and the Massachusetts Sickle Cell Association (MSCA) have joined forces again to identify new research directions aimed at improving pain crisis care for people with sickle cell disease (SCD), a life-threatening, inherited blood disease. This project builds on a prior collaboration between the two organizations focused on SCD pain self-management. This latest project represents a critical next step to enhance care for individuals with SCD.
MHQP and the Massachusetts Sickle Cell Association (MSCA) have joined forces again to identify new research directions aimed at improving pain crisis care for people with sickle cell disease (SCD), a life-threatening, inherited blood disease. This project builds on a prior collaboration between the two organizations focused on SCD pain self-management. This latest project represents a critical next step to enhance care for individuals with SCD.
While it affects people of all races, within the United States, SCD predominantly affects Black individuals, leading to complex challenges at the intersection of healthcare disparities and the need for targeted interventions and systemic changes to ensure equitable care and outcomes. The vaso-occlusive crisis, or “pain crisis,” is a hallmark of SCD, which often manifests as an abrupt onset of severe and debilitating pain.
During the first project, participants highlighted the many barriers to high-quality pain crisis care, including lack of provider knowledge about SCD and how to diagnose and treat pain crises, compounded by inequities and biases in SCD care received at healthcare facilities and a lack of institutional resources. Specifically, patients shared that they often resort to self-care strategies as a way to avoid the racism, discrimination, and low quality care they frequently experience in emergency department settings. This work highlighted the imperative for structural changes in healthcare to improve outcomes and equity for individuals experiencing SCD pain crises.
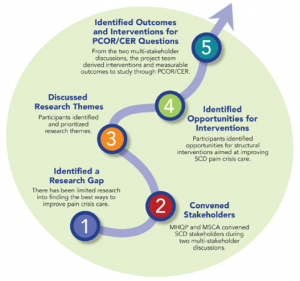
To begin to address these issues, MHQP and the MSCA partnered on a second project to explore directions for future research into pain crisis care through a patient-centered lens.
The project was funded through a Patient-Centered Outcomes Research Institute (PCORI) Eugene Washington PCORI Engagement Award (EASCS #30430), a program that aims to bring more patients, caregivers, clinicians, and other healthcare stakeholders into the research process.
MHQP and MSCA held two convenings in October and December of 2023. The meetings were facilitated by Dr. Lydia Harley Pecker, Assistant Professor of Medicine and Director Young Adult Clinic, Sickle Cell Center for Adults at Johns Hopkins. She was joined by 22 participants – individuals with sickle cell disease, caregivers, providers, researchers, payor representatives, and healthcare administrators – from different parts of the country.
 Based on the learnings from the convenings, MHQP and MSCA created a Roadmap for Future Research Directions into Sickle Cell Disease Pain Crisis Care, which includes stakeholder-identified directions and insights to guide potential research.
Based on the learnings from the convenings, MHQP and MSCA created a Roadmap for Future Research Directions into Sickle Cell Disease Pain Crisis Care, which includes stakeholder-identified directions and insights to guide potential research.
What We Heard
The participants engaged in a robust multi-stakeholder discussion on intervention opportunities for improved pain crisis care, leading to five categories of research: 1) implementing disease-specific education, training, and certification programs for providers and frontline staff; 2) increasing access to providers in emergency department settings who have specialized training related to SCD; 3) fostering community engagement to increase provider empathy and support for individuals with SCD who are seeking care; 4) elevating patient voices; and 5) improving data, transparency, measurement, and accountability.
Implementing Disease-Specific Education, Training, and Certification Programs for Providers and Frontline Staff: Participants stressed the need for comprehensive and ongoing SCD education and training to address not only clinical knowledge gaps, but also the unlearning of harmful stereotypes and biases.
“Emergency physicians need to be updated on the stigmatization of sickle cell disease, so they could prevent biases when they’re treating sickle cell patients.” (Individual with SCD)
“But I would suggest… that it would start with anyone working in the ER area be required to have a minimal educational training related to sickle cell and actually become certified. And that’s not hard to do.” (Provider)
“I think one piece of education that was lacking in my education that feels like it’s lacking in a lot of other providers that I work with, with various other diseases, is the understanding of pain itself and this biopsychosocial contributors to pain.” (Researcher)
Increasing Access to Providers in Emergency Department Settings Who Have Specialized Training Related to SCD: Participants discussed the need for increased access to providers in emergency department settings who have specialized training related to SCD and discussed strategies, such as consulting hematologists upon patient arrival and improving access to infusion centers.
“This would only work in an academic center or a bigger hospital, but as soon as they arrive there, you should call their hematologist, see what they recommend and then go with their care plan.” (Provider)
“I think we have seen that we need more infusion centers, and we need more infusion centers that have longer hours and so if that was something you could wave a magic wand, then you wouldn’t be going to the emergency room, you’d be going to the infusion center with people who know you and can provide that care.” (Caregiver)
Fostering Community Engagement to Increase Provider Empathy and Support for Individuals with SCD Who Are Seeking Care: Participants highlighted the crucial role of empathy in healthcare interactions, emphasizing the need for community engagement activities.
“I had to go to the emergency room… The nurse came [and] my husband told him that I was in a sickle cell crisis. He said, ‘I have no idea about sickle cell but I realized pain is pain,’ so right then and there he connected he understood that I was in pain even though he didn’t understand sickle cell. The emotional connection in the emergency room [is] truly important because as soon as I heard that I relaxed because I knew he was going to deal with me in a particular way.” (Individual with SCD)
“It’s about having physicians and support staff try and create those spaces where they can hear from patients, hear from families can shadow them can understand and try to build connections and community and to build empathy.” (Healthcare administrator)
Elevating Patient Voices: Participants underscored that the voices of individuals with SCD should be elevated through both quantitative and qualitative research methodologies in healthcare settings, research institutions, policy-making bodies, and community forums.
“[The] patient experience [has] to be of quality.” (Provider)
“I feel like doctors prefer more quantitative data with numbers, but what about qualitative data with descriptive factors of, how we feel and how we maneuver the health care system during treatment? Even just applying more patient narratives, storytelling aspects.” (Individual with SCD)
Improving Data Transparency, Measurement, and Accountability: Participants emphasized the importance of institutional support, adherence to established care standards, and public dissemination of data to foster transparency and continuous improvement.
“If there’s no accountability and then things are continuing to happen then there’s really no consequences for these things happening.” (Individual with SCD)
“People will get training, they’ll sit through a training, but they don’t necessarily make it a priority unless your leadership makes it a priority. It makes you say this is important, this is a marker of how well we are doing.” (Payor representative)
“Without data and transparency, we lose the opportunity to have accountability.” (Payor representative)
Where Do We Go From Here?
“We hope this initiative will serve as a vital step towards addressing the stark disparities in SCD research funding,” said Natalya Martins, MHQP’s VP of Programs. “Driving research into SCD pain crisis care is not just a necessity; it is a commitment to improving outcomes, ensuring equitable care, and holding our healthcare system accountable for addressing the unique challenges faced by individuals with SCD.”
“We are optimistic that researchers and stakeholders in the SCD space will utilize this research roadmap to initiate exploration of this understudied topic, viewing it through a patient-centered lens,” shared Jacqueline Haley, Executive Director of MSCA. “In representing individuals with SCD globally, we were excited to collaborate with MHQP on this invaluable initiative, shedding light on a much-needed area. We eagerly anticipate future research partnerships with MHQP.”
“We are delighted to have collaborated for a second time with MSCA,” said Barbra Rabson, CEO of MHQP. “We anticipate an ongoing partnership to pursue the research directions we identified through this work in the near future.”
If you are interested in learning more or getting involved in this important work, please contact Natalya Martins, VP of Programs at MHQP, at nmartins@mhqp.org or Jackie Haley, Executive Director at MSCA, at jacqueline.haley@gbscda.org.
