MHQP and GBSCDA Seek New Research Directions for Sickle Cell Disease Pain Self-Management

(August 2022)
Sickle cell disease (SCD) is an illness that predominantly affects people of color and is characterized by debilitating pain. As with other chronic diseases, self-care is a key strategy for people with SCD to manage the disease and avoid or mitigate pain episodes. Yet, to date, there has been limited study of the most effective, patient-centered approaches to help people with SCD manage their pain outside of clinical settings.
To begin to address this research gap, MHQP partnered with the Greater Boston Sickle Cell Disease Association (GBSCDA) to explore directions for future research through a patient-centered lens.
Underlying Currents
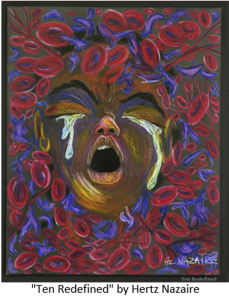 “Our hope is that this effort can begin to address the striking inequities in research funding in our country,” said Natalya Martins, MHQP’s Director of Strategic Initiatives. “We need to recognize the underlying currents of bias and racism at play here. Patients of color regularly experience treatment inequities, and this is especially true for acute and chronic pain, both of which are characteristic of SCD.”
“Our hope is that this effort can begin to address the striking inequities in research funding in our country,” said Natalya Martins, MHQP’s Director of Strategic Initiatives. “We need to recognize the underlying currents of bias and racism at play here. Patients of color regularly experience treatment inequities, and this is especially true for acute and chronic pain, both of which are characteristic of SCD.”
In fact, a 2020 New England Journal of Medicine perspective piece stated: “there may be no population of patients whose health care and outcomes are more affected by racism than those with sickle cell disease.” An orphan disease affecting over 100,000 people nationwide, SCD does not receive funding proportional to that directed to other rare diseases, as documented in this 2020 article published by JAMA.
To deepen our understanding of these issues and generate future patient-centered outcomes research and comparative effectiveness research (PCOR/CER) directions in SCD pain self-management, MHQP and GBSCDA held two convenings in April and June of 2022. The effort was funded through the Patient-Centered Outcomes Research Institute’s (PCORI) Engagement Awards program, a program that aims to bring more patients, caregivers, clinicians, and other healthcare stakeholders into the research process.
The meetings were facilitated by Dr. Lanetta Bronté-Hall, President and CEO of the Foundation for Sickle Cell Disease Research, and included eighteen stakeholders – patients, caregivers, providers, researchers, and policy advocates – from different parts of the country.
What We Heard
Here are just a few of the eye-opening comments we captured from the meetings:
“I think one of the barriers really is the bias against self-management. And what I mean by that is when you’re trying to [get] care from some of the providers, they’re turning to what I’ll term the more traditional approaches… And I think that puts you in a mindset of going away from some of the other strategies that you could use… [For example,] taking supplements at the time of pain – we don’t hear about that. We don’t really hear about nutrition. We don’t hear about those strategies. And that could help prevent some of the pain issues. The focus on the tradition is one of the barriers to [effective] self-management.” [caregiver]
“If someone’s frequently in the emergency department, they’re like, oh, why are you always here, they must not be in pain they’re drug-seeking… And then emergency physicians … they’re not as diverse as our patient population… because of that, you also have issues with cultural competency… Labeling people before you even see them as a drug-seeker [further] delays their care.” [provider]
“One barrier… for going to get pain managed at the hospital is the cost… It’s like, okay, if I go to the emergency room, I have to pay a hundred dollar deductible right off the bat. And then I have to deal with the bill that’s going to come, and I do private insurance through my employer and so it’s like, okay, I’m going to be stuck with that 20%, and ER visits are not cheap.” [patient]
“The resources are lacking at the institutions. I remember talking—I’m in the Baltimore area—I remember talking to a patient and they were raving about, you know, [an] infusion center, but it’s not 24/7. So, I asked, so, what do you do? And she, you know, jokingly said, well, I just decided I’m not going to get sick on the weekends.” [caregiver]
“If I go [to the ER or day hospital], it’s going to be a nightmare. So let me try the Motrin, let me try the Tylenol, let me try the heating pad. None of it works. And you end up… six hours into the pain crisis and it just is worse.” [caregiver]
The Barriers
With these comments as a backdrop, the group identified the most significant barriers that suppress SCD pain self-management:
Mistrust – Provider-patient relationships must be built on trust. Yet, patients and caregivers alike spoke to the deep history of racism and mistreatment that happens in the healthcare system, which has led to many patients with SCD to become distrustful of the healthcare system. This mistrust leads to patients avoiding clinical care for fear of discrimination and causes patients to be less likely to initiative or engage in dialogue about their care and share their knowledge about their disease experience.
Lack of Shared Decision-Making – It is important for providers to engage with patients in the decision-making process and understand why patients make certain pain management and care decisions. However, the patients and caregivers in the meeting shared their feelings that providers do not always consider the patient as a whole person, nor do they value the expertise that patients and caregivers bring to the table. This lack of shared decision-making can cause providers to not tailor self-management practices to meet patient needs.
Inequities and Biases – Although SCD chronic and acute pain can be severe, providers sometimes do not understand patients’ pain or believe that they need medications to manage their pain. In addition, in the context of the opioid crisis and the regulations that followed, many providers became more hesitant to prescribe pain medications. Pain is subjective, so it is susceptible to bias, which leads many patients with SCD to be labelled as “drug-seeking.” These biases can cause providers to be mistrustful of patients’ true motivations and patients to avoid clinical care for fear of discrimination.
Inadequate Patient Education – Patients in the meeting voiced that they need more health education. Specifically, they expressed a desire for more information on how to identify pain triggers and when to seek clinical care. This lack of knowledge may lead to an over-reliance on medications.
Inadequate Institutional Resources – Institutions lack the clinical resources to fully support their patients. Access to care is limited by office hours, behavioral healthcare providers are frequently not on the care team, and community resources are commonly not available to address issues locally.
Low Patient Bandwidth – Patients reported major bandwidth barriers to actively seeking and participating in SCD care. It is a large commitment to manage chronic and acute pain and other SCD complications, and patients often do not have the time, resources, or energy to do so. This can lead to patients being overwhelmed by the decision-making process.
Inadequate Provider Training – Providers noted that they have not been trained to provide alternative care, although patients, caregivers, and providers expressed interest in alternative care strategies. In addition, providers shared that they would like more training on how to best support patients in self-managing their pain. This knowledge gap may lead to an over-reliance on prescribing medications.
Lack of Transitional Care – Many patients with SCD experience an increase in disease complications and the need for health care as they age and during the time of transition to adult care. However, there are often not systems in place to smoothly transition pediatric patients into adult care, leading many patients of transitional age feeling neglected and mistrustful of healthcare system.
Where Do We Go From Here?
Based on the learnings from the convenings and the barriers identified, MHQP and GBSCDA created a Roadmap for Future Research Directions into Sickle Cell Disease Pain Self-Management, which includes stakeholder-identified directions and insights to guide potential research.
“We are hopeful that this research Roadmap will be utilized by researchers and other stakeholders in SCD, to begin to address this understudied topic, through a patient-centered lens,” said Jacqueline Haley, Executive Director of GBSCDA. “On behalf of SCD patients everywhere, we were excited to partner with MHQP for this very valuable work and to bring much needed attention to this topic. We look forward to partnering on future endeavors with MHQP, focusing on improving the general welfare of patients living with SCD.”
“We are thrilled to have had this opportunity to work with GBSCDA,” said MHQP’s CEO Barbra Rabson. “We look forward to a continued partnership and other synergistic efforts to tackle this burdensome disease in the near future.”
If you are interested in learning more or getting involved in this important work, please contact Natalya Martins at nmartins@mhqp.org.
