Tackling Inequities in Pain Assessment and Management
 (August 2022)
(August 2022)
Historically marginalized communities are systematically undertreated for pain, and this issue disproportionately impacts Black women. While this fact is well established by research (1), we know very little about the specific barriers that Black women experience when they seek pain care.
To help identify opportunities to close this research gap and expand our understanding of the underlying causes for biases in pain care, MHQP launched the Pain Inequities Project. We conducted interviews with patients from a variety of racial, ethnic, socioeconomic, and cultural backgrounds who have experienced chronic pain, as well as providers across specialties who treat patients with chronic pain.
Shining a Spotlight on Inequities
What makes pain care unique in contrast to most other maladies is that it is fundamentally subjective. Because of this, it is particularly susceptible to bias, and the patient’s credibility can be called into question. This issue appears to be particularly problematic for Black women. A 58-year-old Black female patient we interviewed summed the patient experience this way:
“It’s because of what I look like. I don’t get treated well and that’s why I stay out of doctors’ offices. Those people with the white coats – they have this thing about who we are and what we’re worth… Something’s gotta give for healthcare and for women and People of Color. It’s bad out there.”
On top of that, healthcare providers are not trained to assess pain and tend to not be as comfortable with issues that cannot be objectively confirmed. A 47-year-old white female provider summed up the provider experience like this:
“Pain is so subjective – [it is] hard to know what it is and where it’s coming from. We’re not trained in multi-factorial aspects of pain and our own bias in how we treat pain.”
Barriers to Effective and Equitable Pain Care
With this context as a backdrop, the project team analyzed the interview results to identify the most common barriers to effective and equitable pain care:
Access – Inadequate access to high quality care is a major barrier to achieving equitable pain care and is inarguably a social risk factor for negative health outcomes. The patients we interviewed discussed several access barriers, including inadequate paid sick time, location/transportation issues, language barriers, and lack of community resources. These issues may contribute to Black patients being disproportionately reliant on the emergency department for their healthcare.
Trust – Provider-patient relationships must be built on trust. Yet, the patients we spoke with pointed to generations of racism and mistreatment at the hands of providers, which has left many communities of color distrustful of the healthcare system.
Connection – It is important for providers to communicate effectively with patients and for patients to feel heard. If providers do not share the same cultural background or speak the same language as their patients, it can be more difficult to connect and build a relationship.
Provider Training – Providers attributed a lack of training and education around pain care as one of the reasons that poor pain assessment and management persists.
Patient Capacity – Interviewees reported major bandwidth barriers to actively seeking and participating in pain care. Patients must balance competing priorities in order to navigate a complex healthcare system and receive care. It is a large commitment to manage chronic pain, and patients often do not have the time, resources, or energy to do so.
Health Literacy – Our healthcare system is extremely complex, which the patients we interviewed report makes it very difficult for them to navigate resources to help them manage their pain and underlying conditions.
Insurance and Financial Resources – We heard from many participants that it can be expensive to treat chronic conditions and manage chronic pain. Even the patients we spoke to who had health insurance worried about the cost of care.
These barriers are intensified for groups that have been historically mistreated by the healthcare system, and especially for Black women, yet inequities in pain assessment and management have not received warranted attention from the research community. MHQP believes that further exploration of these barriers will help to accelerate research and policy agendas needed to eliminate racial inequities in pain care.
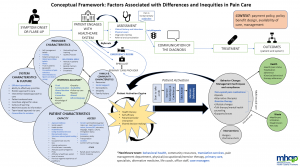
A Conceptual Model
With these barriers as a focal point, the project team developed the following conceptual model to help drive change by presenting a visual map of the factors associated with inequities in pain care. This model illustrates how the barriers prevent patients from receiving a timely diagnosis, establishing effective working alliances with their providers, and becoming an activated participant in their care.
What Can We Do About It?
Pain care is undeniably a health equity issue. When patients are in pain, they are in their most vulnerable state and, more than ever, they deserve the best we have to offer. However, pain care is often inadequate, and Black women carry an unequal burden. For our healthcare system to be truly patient-centered and equitable, we must identify the system-level issues that perpetuate inequities and take proactive steps to address underlying biases.
MHQP is doing all that we can to spark action on this issue. For example, we co-led a project with the Greater Boston Sickle Cell Association designed to identify new directions for research into patient-centered approaches to help people with sickle cell disease self-manage their pain. We look forward to other similar opportunities in the future and welcome your feedback, suggestions, and partnerships on this important work.
———————
- Hoffman & Tarzian, 2001; Hoffman, Trawalter, Axt, and Oliver, 2016
