MHQP Introduces Measured Equity, a Statewide Initiative to Measure Racial and Ethnic Disparities in Patient Experiences
(September 2023)
We can no longer ignore the systemic racial and ethnic disparities in patient experiences that plague our healthcare system. Organizations across the state are taking action to address these disparities, but these complex issues can only be effectively addressed by working collaboratively across organizational lines, not in organizational siloes. At the Health Equity Trends Summit assembled by the Health Equity Compact in June, there was general consensus that reducing disparities requires us to coordinate our efforts for maximum impact, engage the communities and patients we serve, and measure our progress to hold ourselves accountable.
MHQP can help achieve these important goals. We have a long history of catalyzing collaborative measurement between stakeholders in Massachusetts healthcare to help tackle complex challenges such as this that none can solve alone. That’s why we have launched a new statewide initiative we are calling Measured Equity.
Measured Equity will consistently measure and report racial and ethnic disparities in patients’ experiences across the state, establishing a shared measurement and reporting system that will allow participants to identify the systemic issues driving disparities, compare performance across organizations, focus on best practices for organizational improvements, and track progress over time.
Why Patient Experience?
Measured Equity will leverage MHQP’s Patient Experience Survey platform, the only statewide survey of patient experiences in Massachusetts. MHQP has surveyed thousands of patients from primary care practices across the state each year for nearly two decades, using a time-tested instrument and a consistent analytic approach across all systems to create comparable results. In addition to quantitative data, we also capture thousands of narrative comments through which patients illuminate – in their own words – the impact of the biases they experience every day. This feedback provides an authentic view of how patients are actually treated in the healthcare system, allowing us to dive beneath the surface to a deeper understanding of the drivers of disparities to inform interventions.
What’s more, because positive patient experiences are associated with important clinical processes and better outcomes, it is our firm belief that this deeper appreciation of how patients experience healthcare is an essential foundation for addressing disparities across all health outcomes.
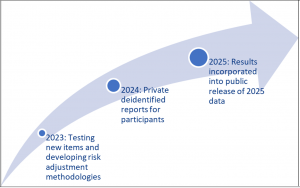
Glidepath to Public Reporting
MHQP and our participating stakeholders will move together toward stratifying data by race and ethnicity in our public reporting of statewide patient experience results, beginning in 2025, as part of our ongoing commitment to equity, transparency and accountability.
 In 2022, we worked with participating organizations and health equity experts to add new demographic questions to the survey to align with the state’s new health equity data standards, as well as questions about social risk, that will enable us to better understand racial and ethnic disparities in care and allow us to stratify results by race and ethnicity in future years. These new questions were included in the 2023 survey.
In 2022, we worked with participating organizations and health equity experts to add new demographic questions to the survey to align with the state’s new health equity data standards, as well as questions about social risk, that will enable us to better understand racial and ethnic disparities in care and allow us to stratify results by race and ethnicity in future years. These new questions were included in the 2023 survey.
This year, we are working with participating organizations, the CHA Health Equity Research Lab, and health equity experts through a collaborative process to test models of social risk-adjustment that account for social risk to ensure fair comparisons across organizations. This methodology will be deployed in our analyses beginning in 2024.
In 2024, we will provide participating organizations private reports which will include comparison vs. de-identified peer groups, utilizing the agreed-upon risk adjustment methodology. This information will not be made public in 2024, so participating organizations will have exclusive access to survey results from the 2023 and 2024 cycle, which will enable them to compare how their organization performed versus peer organizations on measures related to racial and ethnic disparities before we begin to incorporate these metrics in our public reporting of 2025 results.
In 2025, data for all organizations, stratified by race and ethnicity, will be released publicly. This gradual approach will support data verification and encourage collaborative refinement by participating organizations.
Who’s Already On Board
Many of the state’s top organizations partnered with MHQP in the first year of this initiative in 2023:
- Blue Cross Blue Shield of Massachusetts
- Point32Health
- Health New England
- Mass General Brigham
- Tufts Medicine Integrated Network
- Steward Health Care System
In addition, representatives from Boston Medical Center, Cambridge Health Alliance, and MassHealth have contributed their expertise to some of the complex questions related to risk adjustment.
We are currently engaged in conversations about the opportunity to participate in 2024 and will publish the list of participants once it is final. If your organization is not already participating, this is your opportunity to help drive this collective effort to reduce disparities for patients in Massachusetts and “raise all boats” to truly advance health equity across the state.
For more information about Measured Equity, please contact Natalya Martins, MPH, MHQP’s VP of Programs, at nmartins@mhqp.org.
