MHQP Releases Results of “Together for Better Telehealth” Surveys
 (November 2020)
(November 2020)
Several months ago, as the COVID pandemic began to take hold and most interactions between providers and patients moved to computer screens and telephones, MHQP launched an initiative we call “Together for Better Telehealth.” It’s an effort to help clinicians share what they are learning from their telehealth experiences to help the whole profession adapt to this new way of providing care.
In July, we sent a pilot survey to a small network of clinicians. The 130 responses we received from clinicians across a variety of specialties contained many interesting insights and revealed wide variations in the telehealth experiences of healthcare providers across the state. Below are the major themes discovered. You can click on the “+” sign to reveal comments from responders supporting these themes.
- “[I’ve learned] that I’m able to adapt to change in practice more easily than I expected.”
- “I am surprised by how diagnostically comfortable I am when not in the exam room with a patient I am evaluating.”
- “[I’ve learned] that I can learn technology.”
- “I am more flexible than I thought and my skills translate to a telehealth platform.”
- “[I’ve learned] that my history taking skills are very good and most times the physical exam did not change my diagnosis.”
- “I don’t mind telehealth as much as I thought I would.”
- “[This has] validated my realization as a new NP that 95% of info used for diagnosis is based upon what the patient tells me.”
- “I can innovate pretty well! I’m more flexible than I thought!”
- “I/we are an incredibly versatile lot. Our commitment to lifelong learning and constant change in our profession has trained us well for meeting this moment successfully.”
- “It is important to remain flexible and adapt quickly to change because the faster we do this, the better we can serve our patients. I learned that I am very quick to pick up on technology changes.”
- “I love learning about my patients, but I am easily exhausted by the amount of eye contact one has during a Zoom call!”
- “I need to work harder to remain in the moment and focused on my clients.”
- “[I’ve learned] that I’m getting old.”
- “I miss working collaboratively and in person with a team.”
- “It’s difficult, I don’t work well working in isolation.”
- “[I] request verbal feedback to ensure important information was understood.”
- “[I] ask more clarifying questions on the patient experience.”
- “[I am] a bit more active and directive.”
- “[I] speak slower and more distinctly and have more than one person on the call if they are elderly.”
- “For young kids, I ask parents to perform some of the exam and report.”
- “I have become more adept at being on time with my visits.”
- “I try to get as much information from the patient by instructing them how to physically check things in their bodies! I had a sick patient with COVID who I had lie down so I could count his respiratory rate by watching his abdomen. Vent the next day as I insisted the day of the telehealth visit that he got to the hospital!”
- “When needed, we bring patients into the office for visits despite COVID; if needed based on the chief complaint or if something is identified in the virtual visit that needs physical exam.”
- “[I’m] asking them to lay their hands on themselves (patient assisted exam) and conducting more thorough history-taking to make up for lack of physical exam.”
- “I have tried to communicate using a more expressive tone of voice and more expressive facial reactions to better convey my message.”
- “[I ask] more specific questions and use diagnostic equipment at their homes like Vital signs and blood sugar or apple watch monitors.”
- “I have the family take photos prior to visit to allow review.”
- “Someone else on the visit can facilitate things, i.e., push on a person’s legs so I can see if there is pitting edema.”
- “I ask them to describe what I might see if I was with them. Are you sitting? where are you sitting? where are your feet? on the ground? how about your shoulders? Etc.”
- “Telehealth has its place but also limitations. I learned that I can use it for certain problems but not all.”
- “[I’ve lost] the joy of this work.”
- “I am still seeing many patients in the office – not being able to examine a patient ties my hands as a clinician and limits the usefulness of most visits, with the exception of most visits regarding mental health issues.”
- “I thought it would feel essentially the same, but it feels more disconnected and less socially meaningful to have to see patients in this way.”
- “Telehealth does not work for me.”
- “Not doing telehealth. We need to see patients in the office. We are ophthalmology.”
- “Very inefficient in terms of # patients per hour relative to office practice.”
- “I hate telehealth for well visits.”
- “I avoid telehealth visits in patients where an exam is needed.”
- “I am a surgeon. Telehealth has a very limited role for individuals that rely so much on physical exam. It is not a real encounter in my perspective.”
- “I find it challenging to manage certain conditions such as various rashes via telehealth.”
- “There are challenges bringing video technology to the very elderly.”
- “I loved learning that a patient of mine is an avid birder! I would never have known as he has never mentioned it, but I saw all of his paraphernalia during a telehealth visit and we had a lovely discussion about this hobby of his.”
- “[I’ve been surprised by] the intimacy in the stories.”
- “It is helpful to see patients in their own homes, and sometimes a family member or caregiver can help make up for my inability to physically examine the patient.”
- “I have had several encounters in which patients seemed more comfortable, in their home environment.”
- “I feel I can have more casual conversation on telehealth.”
- “Seeing patient environments has a lot of value that I did not expect. For example, I have a patient I’ve known for almost 2 years. I had no I idea she was a hoarder until I saw her via telehealth at home.”
- “Patients open up and tell me all sorts of things and are more comfortable about how they feel in their own houses.”
- “I see my shy patients blossom on video in the comfort of their own home.”
- “Some patients appear more comfortable and able to let down their personal walls.”
- “Many patients seem more honest and less tense when discussing stressors, anxiety, and depression from the comfort of their own homes.”
- “Some really young kids…bring me their favorite belongings to see and ‘show’ me their room.”
- “I got insight into a patient’s home environment and ability to do things such as see medications they have at home to help in treatment.”
- “I really enjoy seeing patients in their own home. I’ve known most of them for decades and so getting to see their pets and their hobbies and they show me the views from their windows. Very enjoyable.”
- “I found that seeing patients in their homes and sometimes even meeting their pets created a more personal dynamic.”
- “I feel I can have more casual conversation on telehealth.”
- “[I’ve learned] that I like the human contact and being able to be in the same room with my patients, allowing for small talk sometimes…which helps me be a better physician.”
- “Can’t draw pictures very easily for them to understand pathophysiology, anatomy etc.”
- “Emotions expressed are worrisome since I have poor visuals.”
- “I miss the ability to show compassion through holding a hand or giving a hug as appropriate.”
- “I like being able to see and read patients’ and parents faces.”
- “I prefer to see patients in person.”
- “Currently, I am seeing approximately 75% of my volume in person.”
- “I am a more of a hands-on physician.”
- “I enjoy being physically in the room with my patients.”
- “90% of what I do is based on a ‘connection’ and I can connect with most people by video quite well.”
- “I miss face-to-face communication.”
- “With certain follow-up visits it makes things easier for me as a clinician. It also makes it easy on the patient – no need to find parking, get to office, etc.”
- “My transgender patients feel infinitely more comfortable having telehealth appointments because it allows them to relax more in the setting of their choosing. All of my patients have felt this way, but my transgender patients especially because accessing healthcare can be traumatizing for them.”
- “A 90+ year old patient and her family and caretakers [were] safely at home while managing the technology to get the care they needed.”
- “Patients are more happy probably because they are not going through the stress of driving to clinic, waiting in exam rooms, etc. They are much more comfortable.”
- “I find it is helpful for younger patients with basic problems and time constraints.”
- “Stress on the entire system can be lessened when selected patients are handled by telehealth for selected visits.”
- “Several post-hospitalization follow-ups are performed virtually when the patient would not have been able to come into office otherwise due to transportation or weakness.”
- “I like it for postop patients who are doing well. It saves them time and money.”
- “Older patients, who can actually manage telehealth, are excited to talk to a familiar face.”
- “I see a lot of depressed patients. I think telehealth helps them open up more.”
- “For diabetes patients whose insulin pumps are linked for data download, it is very effective.”
- “I saw a mom with post-partum depression. It was great for her that she didn’t have to come into the office and bring the new baby during a pandemic.”
- “I feel it helps the immobile and infirm get medical care.”
- “I would like to know from the clinical fields in general whether engaging in telehealth through an online platform has been able to reach all families across diverse economic circumstances and what they’re doing to ensure equitable access to quality care through devices.”
- “For patients who can’t do video, I miss seeing them altogether.”
- “[I’m] seeing huge disparity in English speaking and non-English speaking access to telehealth at the outset. Not technology based, rather the outreach has been in English and not hit the communities of other languages. More evolving strategies needed. Social determinants of health come into play, but everyone should be able to get access. “
- “Hard sometimes when others in the room to be sure patient is being honest.”
- “Some patients do not feel they have a safe or private place to have a telehealth visit.”
- “Some patients have a harder time opening up. I’d say the biggest issue is around patients having access to reliable technology and a safe space to talk.”
- “[It’s challenging to] have private conversations with teens.”
- “Patient could physically show me their meds and how they had them set up to dispense to themselves.”
- “Patients love it. More compliance and minimal rate of no shows.”
- “We can solve some simple situations easy and can save patients travel.”
- “I have been pleasantly surprised at how easy it is to instruct patients on self-injection. I thought it would have been much more difficult.”
- “I have liked the increased ability to connect with the home care nurses when they are actually visiting the patient – so they become my eyes.”
- “I thought it would be impersonal, but it has not been my experience. Visits go smoother and quicker. Patients have less time waiting for the clinician to see them. Also, much more private than coming into the office.
- “[I’m surprised by] the convenience and the increased engagement with patients who used to ‘no show’”
- “I did not think I would like telehealth, but I love it. I have met family members, engaged family in treatment, and even gotten a tour of a patient’s new apartment. It’s really shifted the relationship to be less hierarchical and more inclusive of those with disabilities or other barriers to care.”
- “I am more comfortable asking difficult/private questions.”
- “Significantly decreased no-shows and boosted caseload.”
- “[I] realized low yield parts of my in-person workflow.”
- “I found that med-reconciliation was more accurate when done by telehealth/phone. Patients can collect meds and read them off.”
- “I’m more efficient through telehealth, seem to have less room for small talk with patients.”
- “I am able to speak better without the mask.”
- “Without the exam, office paperwork, and other procedures, there is actually more time to talk.”
- “I tend to do better record review on telehealth particularly on EPIC shops.”
- “The attention to history taking is increased due to the inability to get a physical exam.”
- “The patient history is typically more important than the exam. We were taught that in med school, and we all relearned that in COVID.”
- “[The] patient narrative, in contrast to physical exam, is 90% of what is needed for dealing with most problems.”
We then built upon the results of the pilot survey with a “Wave 2” survey (fielded between August 27 and September 9, n = 194) and a “Wave 3” survey (fielded between September 21 and October 16, n = 210) through which we sought practical solutions, useful ideas, tips and tricks for how to make telehealth better in the subject areas listed below. For each subject, we asked a “quantitative” question and offered an opportunity for respondents to provide “qualitative” comments. Click on the “+” sign to reveal the data and comments for each area.
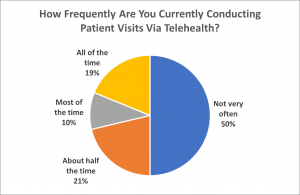
Comments:
- “It changes depending on who I’m seeing. I foresee more online visits as kids go back to school. Telehealth visits have fallen off as the unmet demand for physicals deferred is being addressed as patients are more willing to come into the office.”
- “Choice should be based on patient preference.”
- “In person is much more efficient.”
- “Would prefer more video visits, but it is not being offered or stressed with patients as much as I would like it to be.”
- “I provide a great deal of phone care but remain uncomfortable billing for the majority of these interactions because patients have become accustomed to receiving this care without a charge.”
- “Would actually like to do more video visits, but recently patients have been much more interested in being seen in person.”
- “I think video visits are the way of the future, but the connectivity needs to be greatly improved in order to be efficient and timely in completing these visits.”
- “Our patients have significant impediments to video with band width and connectivity issue in rural area. Since there is no evidence that video is superior to or adds anything significantly more to the visit, the differential reimbursement is creating a disadvantage for those without resources or living in areas with poor internet connectivity.”
- “Telehealth has been very very helpful to maintain continuity of care for our patients.”
- “I have been hesitant to perform to many video as they don’t appear any more effective than a good phone conversation. It is only financial that we will eventually need to convert potentially to this format. Currently the workflow to have patients ready and checked in without provider waiting or troubleshooting is not efficient.”
- “This has been challenging and refreshing also. With the proper triage, appropriate scheduling and making sure the technology is working both sides, telehealth is a blessing much needed in primary care. This should carry on from now on, at the same level we perform now, not just because of the pandemic. This way of practice is modern, fresh and needed reform in our practice. It helps to get patient care faster and more efficient. Based on my experience at least half of the primary care visits don’t need the patient to be at the office. And doing it right the interaction with the patients is wonderful. They show me around their house, they feel more comfortable talking about any issue, they don’t need to take time off from their work or wait in waiting rooms. I love it!”
- “Phone calls are secondary for patients without the ability to do video or for patients with ESL and need of translator.”
- “We are a small municipal agency and have been meeting people outdoors when we can.”
- “Video capability remains very complicated and time-consuming due to the platform my organization has chosen to use.”
- “My patients prefer in person visits.”
- “New patients often want an in-person meeting if they respond well to treatment. Then back to telemedicine for safety. Especially among elder patients.”
- “It changes based on evolving state policy.”
- “Internet and video are not available, complicated and/or not smooth to use for most of our clients.”
- “I am very high risk and isolating at home. Telehealth has helped me stay in touch with patients. Patients who are savvy send me e-mail and I will return calls or set up a formal telehealth visit depending on the issue.”
- “Phone is due to poor internet connection or lack of internet, a patient with a trauma history where video is triggering and uncomfortable, or a patient with social anxiety that’s intensified by video.”
- “The only time we use phone is when there is a significant tech issue.”
- “Overall, patients seem much more engaged in Behavioral Health video visits. Somehow, they manage to be both more intimate but less anxiety provoking for patients.”
- “I have been using video since the beginning and it has been great for the patients and families; I have access to details, to family and history that I didn’t have in-person. Family has been more engaged. And is safe for patient, family and clinician.”
- “I try my best to have patients engage in video visits as I find that it offers more information (visual) and I am better able to remain engaged.”
Please share any criteria or strategies you use to determine when it’s best to have a phone vs. video vs. in-person visit:
- “Patient is able to track key health parameters required for assessment (e.g., blood pressure, weight) at home. 2) Patient has available technology (video preferred, phone is last resort) 3) Patient concern re: the safety of in-person visit during pandemic 4) Provider concern that in-person visit is needed to assess the patient. 5) Patient preference to have in-person visit.”
- “Chronic disease, anxiety/depression, rashes lend themselves to telehealth. Anything needing exam (e.g. abdominal pain, ear pain) needs in-person.”
- “Does the patient need vaccines or tests done? Does the patients need a physical exam that can’t be performed by telehealth? Does the patient want an in person visit? After initial assessment, do I feel an in person visit is needed for delivery of appropriate care? If answer to any of the above is yes, then do an in person visit. If not, do virtual.”
- “GYN: If they would benefit from an exam or need a procedure, we are trying hard to capture their testing, radiology tests before an initial visit where we can better complete the consult. Follow up visits to assess success of treatments and many post op visits can be done by phone. OB: we are seeing patients almost as regularly but using televisits for many of the early visits and doing more in person visits at the end of pregnancy largely for blood pressure monitoring and monitoring of higher risk pregnancies.”
- “Hard of hearing needs in person; no BP or weight reading in someone over 40 or with Hypertension/Obesity needs in person; psych issues do well virtually.”
- “I look at phone visits for elderly non tech savvy patients who I need to have extended treatment plan discussions with. I look at video visits for issues like acne, initial rash evaluation, eczema or psoriasis initial visits. I prefer ‘seeing’ it in person but it depends on patient’s availability and preference.”
- “I want to offer video as first option. Younger people tend to do it. Older patients seem to want to come in person. Most people want to come in person for their “physical” even though I think it unnecessary. It is mostly driven by patient preference.”
- “If the patient requests or I need to actually listen to lungs, heart, etc., I will see in person. Many of my patients are homeless, no phones which make in person visits mandatory.”
- “In person for things like looking in ears, pelvic exam needs. Pretty much everything else can be done via video. It works especially well for behavioral health issues as patients feel secure in their own habitats talking via video.”
- “In person only for clients unable to access telemedicine effectively (one elderly client , 2 young children). In person occurs out of doors, with masks, with only one exception. That one client can not tolerate being out in the heat with a mask and is seen indoors at a 12 foot distance in the waiting room of our closed practice.”
- “In-person may be necessary in some crisis situations, but telehealth is working swimmingly. I highly recommend video in all cases where the client is capable of and has access to the technology. You only glean so much about a client’s presentation, mental status, and so on during a phone call. At least in a video you can have eyes on the client and can see body language as well as hear their voice.”
- “Looking at rashes via video or on My Chart is not the same as seeing and feeling the rash in the office in 80% of cases. In person is always best with children, as we cannot assess abdomens, hearts, lungs and most rashes via video. Also, it is great for the children to get out of the home.”
- “No phone visits, since they don’t count in productivity. I would love to do more of these with my elderly patients as it worked well during initial COVID confinement.”
- “Office visit for unique clinical problems, language issues, reliability issues.”
- “Only if very high covid risk would I do video or if something simple like going over MRI.”
- “Patient choice with clinician’s input regarding safety and clinical need for visual and other in person information.”
- “Patients that need a lot of manual treatment should be seen in person is able. Patients that need more education and lifestyle modification can be seen via phone or video. Patients requiring exercise can be seen in person or video.”
- “Phone calls as a medium do not have sufficient data to do complex therapeutic work. Video does. In-person reserved for patients with an urgent/emergent problem who should not be referred to the ER.”
- “Phone is the default, in person for something that needs to be examined in person (ie neurologic exam, vaginal exam), video for rashes or patients who are motivated to figure it out!”
- “Phone when patient says eyes look normal to them but just has symptoms . Video when eye is red or other signs . In office when the need to use bio microscope or needs dilation due to flashes or new floaters or loss of vision.”
- “Scheduled lab follow up, no new issues, CPE for healthy person, mood/psych issue will try to conduct video visit. Problems that require more extensive examination (abdominal pain, significant MSK pain) or problems that may have dangerous etiologies (chest pain, dyspnea) not appropriate for phone.”
- “Straightforward post op patients can almost always be televisits (phone or video). I always prefer video unless the patient cannot do a video visit – then if appropriate I will do a phone visit.”
- “Technology available to my patients is the only reason I select phone over video – would always prefer video. In person most related to high complexity or need for in person physical exam.”
- “This is patient driven based on availability of smart phone, tablet, computer and ability to use technology.”
- “Video has been great for medication checks (adhd or anxiety/depression), or if kids are away at college and can’t come into the office.”
- “Video is preferable unless patient is technologically incapable (which is almost all geriatric patients).”
- “Video is very difficult for elderly patients. Video through Epic hard for everyone. Using Doximity or just face time when possible. Find the phone just as good as video and in some ways less distracting.”
- “Video visits for patients that have potential symptoms of COVID, inability to present to office due to medical frailty or transportation issues or for patients that experience extreme anxiety in being out in public settings during the pandemic.”
- “We do all visits as a televisit first, and use that to determine if a patient needs to be seen in person. If a patient needs medication teaching (e.g., insulin) or complex medication reconciliation that can’t be done via video, we do a one time clinic visit and then follow up via phone.”
- “We have a standard triage system across the system that uses a red, yellow, red approach to book appointment. Green – just book immediately for telemedicine. Yellow – ask more questions, can go either or. Red – definitely book face to face or send immediately to a nurse for triage.”
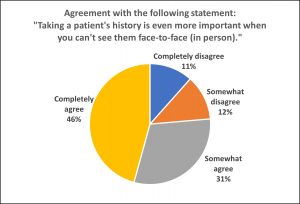
Comments:
- “The history is crucial in all scenarios – for the more cerebral specialties (i.e., Internal medicine), it is largely what drives diagnostic evaluation and treatment.”
- “Taking a patient’s history is always important.”
- “History is history, regardless of whether patient in person or not.”
- “Most patients are at ease talking over the phone.”
- “A good history is not usually dependent on immediate presence.”
- “A patient’s history has always been important to me and my practice. I use a similar/standard assessment. Sometimes I’m better able to understand their life by how their house looks/controllability of their environment, etc. and this actually reduces some need for questions.”
- “It is the same as in person.”
- “I see them face-to-face on the video calls. I think in some ways it’s better – they are dressed and in their own environment.”
- “It is important for both.”
- “I say somewhat because 90% of the diagnosis comes from the history anyway. Sometimes you get more detailed history to decide what is causing belly pain but normally an exam is needed.”
- “It is easier to read body language and expression when a person is in front of you.”
- “Taking a good history is always important although possibly a little more important with telehealth.”
- “I’m a BIG fan of the history and find it is ALWAYS central.”
- “Online medical histories can be filled out by the patient before the meeting.”
- “Taking a client’s history is important when meeting in person and via telehealth/phone sessions, but there can be visual cues that are harder to gauge or determine over video.”
- “People are quite open to talking about their lives, symptoms and health when they are comfortable in their own homes. Even more than when they are in the office.”
- “Taking a history is the most important thing you can do to deliver high quality healthcare virtually or in-person.”
- “Yet we need to understand that direct reporting is not always reliable.”
- “You have to know the history to know where you are going.”
- “A patient’s history is always important regardless if it’s “face-to-face” or via telehealth.”
- “I can take the same history with either office, virtual or phone visit. Taking a proper history is vital always, it should have nothing to do with the type of visit. A provider who doesn’t believe in taking proper medical history should find another job.”
- “Patients also feel listened to when you take a detail history.”
- “In-person allows me to read my patients’ body language. If this is not possible, the history taking needs to be even more detailed than it already is.”
Please share any strategies you have used to ensure you get a complete patient history via telehealth:
- “Allow as much time as needed for each appointment (not scheduling visits back to back).”
- “Ask more probing questions and spend extra time on that.”
- “Ask questions and listen to your patient’s answers. There is so much going on behind closed doors and the only way to get the information is it ask questions. People typically open up more when you’re the one asking the questions which in turns makes them feel important and that you’re listening.”
- “Attempt to read all referring provider’s notes beforehand. Take the time that would normally be used for hands-on objective data collection and use it for conversation/history taking.”
- “Chatting with our (elderly) patients first, and the family, staff members reveals quite a bit, ~50% of your HPI/ROS in the initial conversation, then delve into specific more focused questions.”
- “Focus your inquiry on embellishing what the patient initially presents then expand to questions to help with rule outs.”
- “I actually think this goes better on telehealth because the patient is focused on the verbal exchange and not thinking that a physical exam will reveal everything, so they’re more linear and descriptive with their history.”
- “I ask them detailed questions about duration, evolution, new hygiene habits, meds. It takes more time.”
- “I find it easier, unless they have distractions at home.”
- “I make sure to ask every question and repeat patient answers back to them to make sure I am getting all the details.”
- “I try to write down all items I need to address at televisit beforehand.”
- “It actually seems more natural to engage in the computer and past medical records as you’re talking to the patient, jotting notes on the computer while taking history.”
- “It can be distracting to be using the technology – trying to stick to tried and true interview flows has helped.”
- “Let the patient talk!”
- “More attention is paid to hospital discharge summaries and other extraneous sources of client information.”
- “More structured intake form.”
- “Nothing special needed, we talk. An advantage with telehealth, if we’re at home, is that we can see each other, no masks! And make personal contact, reference something more personal, which puts the person at east – the dog barking, the kids running around, etc. For history I fail to see any barrier with telehealth vs in person.”
- “Patient history is a conversation and given that my patient population is pediatric and my parents are young(er) than most providers! We have no issues obtaining a history. In some cases I get more from the child as they might take the phone and answer questions without their parent interrupting!”
- “Prechart and write all my questions as well as prior relevant lab results or specialty visits.”
- “Relationship and already knowing the person is the most important factor here if telephone only. Harder to do this if meeting each other for the first time, but these are exactly the skills we have already developed in primary care.”
- “Spend adequate time on telehealth to get full history. Pre-sent questionnaires. Medical assistant support to pre-call patient to update histories, med reconciliation.”
- “Take my time and listen without interrupting, same as in person.”
- “They are near their pill bottles, so med rec is actually more accurate; easier access to people they live with for additional history; we use medical assistants to gather standard information and updated information before the provider ‘enters.’”
- “This works better with telehealth since there is no face mask/shield and conversation is more candid and clear with patient.”
- “Trying to encourage a dialogue and keep letting the patient speak as much as possible.”
- “Utilizing rooming MA. Using family member that may be present especially older population. Having them look up medication pill bottles.”
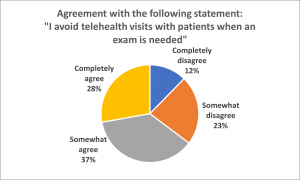
Comments:
- “A fair bit of examination can be done on a high quality video visit.”
- “A family or staff member can help (Assisted Living Facility), this is an option I’ve used successfully all the time of late.”
- “A lot can be inferred by just observing.”
- “Any skin lesions (for excision) can be seen virtually pretty well and diagnosed and planned for surgically (usually).”
- “As a dermatologist, I can do most of the exam via photos or video.”
- “Evaluation is compromised with telehealth.”
- “Exam is very difficult over video, so I have been limited in what parts of the exam I have tried virtually.”
- “Exam remains fairly limited by telemedicine. As a pediatrician, it is particularly hard for toddlers and babies who are unable to remain still.”
- “For dermatology, visual in person is usually needed.”
- “I have found that I am able to instruct the patient through much of what I would do in the clinic. Obviously certain hands on techniques cannot be used, but with certain modifications and specific instructions to the patient, I can often still get the information that I need.”
- “I have used techniques to guide the patient to do things that would help with determining if the patient will need to be seen in person.”
- “I try to avoid televisits if it’s obvious the patient needs an exam, but sometimes people refuse in-person visits and this is the only option to a) triage acuity and b) try to convince them to see a provider in person.”
- “If a physical exam is needed, patient needs to be seen.”
- “In orthopedics, the physical exam is such a vital piece of the visit. Virtual visits limit this aspect of the visit.”
- “It depends on the type of exam. There is a lot that can be done via video. Phone visit is useless and if need for exam should not even be allowed to book. But it is possible to book a video visit to go through a good history and update issues and if I identify there is need for office visit then I can book as follow up.”
- “It is very hard to get patients to demonstrate edema. Can’t hear lungs. Volume status can be tough.”
- “Most of the exam is done for confirmation of suspected diagnosis after a thorough history taking. Engaging the patient in an exam is usually adequate, even for some musculoskeletal exam, abdominal exams, etc. There are relatively few things (inside ears, pelvic exams) that cannot be done effectively via telehealth.”
- “Need to see in person, picture or video are less clear.”
- “Obviously, if a pap exam is needed we can’t do that virtually so we can defer and do the rest of the visit.”
- “Ok to do if limited exam is needed. Patient can also upload pictures pre-visit if appropriate.”
- “Small rashes, local infections are okay.”
- “There are elements of physical exam that I can do virtually, with guidance of patients/family.”
- “There are some clinical conditions when an exam is indicated but can still work it out virtually through the use of pictures or patient/family helping to show physical findings.”
- “There is plenty that can done via observation over phone; rashes, joint swelling, breathing struggles, etc.”
- “You can actually do a lot of the physical exam over the phone with cooperative patients and helpful parents. Augmenting throat exams with photos they can text to me also helps. Rashes can be seen over the phone quite well as can chest exams and even belly exams when properly coached.”
- “You can get some assessment on video, especially general appearance, skin mouth and throat. Can see how their breathing can see their joints. See how they are moving.”
- “You can still accomplish a portion of the visit virtually, even if an in-person exam is required. Some exam elements are possible over video, as well.”
Please share any strategies or techniques you have used to make virtual exams easier or more effective:
- “Have patients palpate areas on the screen, do remote bp checks and temps using home meters, talk to family members.”
- “Have a second person present to help with camera work helps a lot.”
- “I correspond with patients via email and request them to send clinical photos of their rashes or lesions prior to the appointment.”
- “I have patients press on body areas to see if it’s tender, guide them for a musculoskeletal exam and send pictures on my chart of rashes for closer look.”
- “I have the patient help with the exam as much as they can. And to have a spouse/son/daughter etc. help out if they can. Usually the people closest to the patient know if something is wrong and they typically speak up.”
- “I have them open their mouths at the screen, take off their shirts to see their backs, check out hands and feet, evaluate for rashes, observe behavior.”
- “I think about what I really need to see or hear. For pediatrics much of the PE is the general exam. I’ve learned to look at babies’ thighs and cheeks and skin tone to judge weight and nutritional status. For cervical lymph node exam, I advise the parent we are looking for ‘walnuts’ rather than ‘soft meatballs,’ the latter being pretty common and not a concern.”
- “If home bound and have home care nurses, I coordinate with the home care nurse so they do the exam.”
- “Instruct patients in self-palpation send photos in advance of virtual visit.”
- “Instructing patient to push on areas, change the angle of camera for viewing, and use of smart watches/smart phone health data when able.”
- “Natural lighting makes a big difference – so sit by a window.”
- “Our triage team supports set up with videos. We use Zoom in behavioral health and many patients are now familiar with this application. I have post-it notes telling patients they need to ‘join audio.’”
- “Pictures work better for skin exams than video. Ask for picture before video visit.”
- “Request patient to check their vitals ahead of time.”
- “Sending photo rather than streaming video has better image quality.”
- “Sending photos prior for any incisions/skin issues. Having virtual rooming, so patients are ready to have the appointment in a quiet, private room.”
- “Talk with patient/family member first to run thru some basic steps. Discuss lighting, may need to close shades to better see what is happening in encounter. Turn TV off. I have also taught some palpation techniques, i.e., a family member learned recently how to palpate a pedal pulse on her 86 year old mother. Show them how to turn camera around so they can see what I see, yields better physical exam.”
- “Teach the patient how to do an exam on themselves. Have others hold the phone to do exam such as skin exam. Have them flip the camera so they can see what they are filming.”
- “The patient can help with some of the exam, i.e., pushing on their abdomen or tugging on their ear.”
- “Try as best as possible to demonstrate exam techniques to patient.”
- “Video exams are lower yield than I thought they would be. Sometimes it seems that the patient actually needs a holder for their device or another person to assist.”
- “Virtual exam training is available from Mayo Clinic.”
- “With creative thinking we can devise a way to figure out how to do or plan most anything. I studied online other models of practicing virtual telehealth before doing it – as in how to do exams, ask questions, dress, posture, comb hair, and act. It was helpful.”
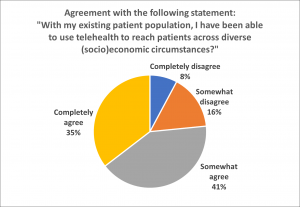
Comments:
- “All my clients have access to a telephone, though very few have video capability or knowledge of how to use it.”
- “Elderly and English as a second language and low socioeconomic patients often cannot engage in virtual appts. No or low access to WiFi and technologies needed. Or else, low tech literacy to set up the apps/programs.”
- “Elderly, underserved and immigrant patients are suffering. We need to bridge the gap urgently.”
- “Hard for really elderly to get on phone. End up needing to have someone else help.”
- “I have been surprised that even the most limited patients or most disadvantaged socioeconomically have the ability to have a video visit on their phone. And I often learn things by seeing them in their home or typical environment.”
- “It has been difficult to use telehealth with my patients of lower SES. I have had a few patients unable to participate as they did not have a smart phone, computer, or access to WIFI.”
- “It is hard to reach patients via telehealth who are working and those who do not have access to internet.”
- “It is impossible for elderly, non-English-speaking patients to do video visits (they don’t have email or a computer, and aren’t comfortable with instructions). Likewise, many of my less privileged patients do not have unlimited minutes/data and therefore can’t waste them to talk to me. This is most of my patient population, so it has been a challenge.”
- “Lack of technology can make video visits challenging for those in lower socioeconomic circumstances.”
- “Many of my low income patients do not have internet access and access to a computer or smart phone.”
- “Many of my patients live far, they don’t have a car, they have kids at home, they can’t take time off work… and it has been wonderful to provide this service. Many of my elderlies have family members helping set up the virtual visit from home. Very positive response from all!”
- “More limited reach to older population who are not as comfortable with technology. More limited reach to lower SES due to limited access to technology.”
- “Most homeless people don’t have phones.”
- “Our most at risk patients are now engaged in care due to the ease of telehealth when previously they have not been able to leave work to come in for care!”
- “Patients with language, literacy, cognitive, issues and low socioeconomic backgrounds have difficult access.”
- “Several of my families don’t have easy transportation access, options for other children in house to be watched while one goes to a visit.”
- “Some patients have internet issues, disabilities mainly hearing impaired patients, group home patients.”
- “Some people do not have smart phones, tablets or computers so I am unable to engage them with video visits.”
- “Telehealth allows greater equity to patient population when they do not have to worry about getting to an office.”
- “Telehealth increases access for everyone.”
- “Telehealth is highly depending on the patient or family member having technical competence and adequate equipment.”
- “The more economically disadvantaged a client is, the less likely she or he will have access to a computer, e.g., Zoom or Google Hangouts. More should be done to educate clients however in the use of their smart phone which most people don’t realize is in fact a handheld computer with video capability.”
- “WIFI is spotty in rural areas.”
Please share any strategies you can suggest for ensuring equitable access to care via telehealth:
- “A really easy to use video connection would be great.”
- “Biggest barriers are general fluency with technology and reliable broadband access. Hard to solve at individual level.”
- “Continue allowing telehealth across the board for all patients!!!!!!!”
- “Delivery or provision of devices and WiFi hotspots to pts who don’t have them.”
- “Encouraging use of low bandwidth video options; measuring the problem; implementing solutions to address digital inequity – virtual outposts in neighborhoods to provide access, partnering across industries to supply internet service, etc.”
- “Extend the office hours so that family members are available at home, in the evenings.”
- “Flexibility helps – sometimes there are technical glitches and I end up being IT support also but I have been surprised how almost everyone has the ability to do a face-to-face visit on their phone.”
- “From my bilingual speaking MA, she noticed that it is hard for non English patient to navigate through mychart because they can not read English. She has learned how to go over step-by-step over the phone how to get onto the visits. It helps the patient, but takes a lot of time.”
- “Help patients with transportation issues – has helped for patients on hospice when family have concerns.”
- “I make home visits to accommodate patients.”
- “I think we do our patients a disservice when we assume that things like language or income barriers make video visits less possible. Almost all young and middle aged patients have a phone with video capability, and when coached we’ve been able to do it. It is the elderly and unstably housed who have the most barriers.”
- “I wish there were vouchers/prescriptions for internet and video phones so everyone could access. I’m sure a lot of money has been saved on “transportation fees.” Would be nice if there was a video/internet service for patients in need.”
- “Increase availability of free hot spots in the community.”
- “Keep telephone paid at the same rate as video and keep that at the same rate as an office visit for Primary Care (at a minimum).”
- “Kiosks in subsidized housing, public buildings, community centers etc should be set up for internet access and video visits.”
- “Mandate that all insurers, public and private, pay for telehealth on par with in person visits.”
- “Rural public libraries have extended wifi signal in their parking lots. I have used this venue a few times.”
- “Smart phone or IPad device for geriatric population to stay connected with their providers.”
- “This is a fabulous way to enhance care for lower SES populations and people with many medical issues or psych issues that make getting to the office challenging. My no show rate has dropped a lot doing video visits. Most patients seem to have phones for use so this is working for them since they can access the telehealth platform on the phone.”
- “Video visits should be as simple as answering a facetime video for patients. We should have a bunch of steps to ensure privacy, but patients should just get a message and press accept. there is too many tech steps and too many problems with microphones or cameras off. If the apps cannot be more patient friendly, we need concerted time and funding to teach patients how to set up and use this.”
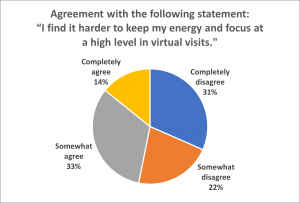
Comments:
- “A full day of televisits does seem somewhat more tiresome than a day full of in-person consultations. That said, televisits tend to be more focused and an efficient use of time.”
- “All day televisits is awful.”
- “Before, there was downtime between patients when I moved into the “pod” to chat with front staff, MAs, med students, etc. Now, I’m just a telemarketer.”
- “Both video and in-person visits have been more draining during the pandemic. I am not sure that virtual visits are any worse than in-person.”
- “Feels more like a performance than a traditional visit.”
- “Focus and energy is much better, lack of distractions.”
- “Gets harder as day goes on!”
- “Going back and forth between in person and virtual visits can be challenging. interestingly, I feel more pressure to be exactly on time for virtual visits but less so when the patient is in the office.”
- “I actually enjoy it much more than I thought I would. It’s like an image-based board exam every visit.”
- “I am able to schedule breaks during the day.”
- “I am not used to sitting on the computer all day. It is draining at times. Additionally, I have chronic dry eye which seems worse now, which I assume is partly due to increased screen time.”
- “I feel more easily distracted – especially if I’m sitting at my own computer.”
- “I find it fascinating to see pediatric patients in their home environments and sometimes it feels more connected because of this. I find the virtual visits invigorating most of the time.”
- “I find it requires almost a higher level of focus and energy because we don’t have anyone to help us. It is quite tiring.”
- “I find no difference in my energy and focus of that when I have in person visit.”
- “I find that some of my clients are distracted by their environment which can sometimes distract me.”
- “I like being able to do more of the computer work (i.e., entering orders, referrals) after I hang up with the patient, and I find myself satisfied that I’ve been able to close more charts in real time.”
- “In a way, it makes visits more focused for myself and patients.”
- “In fact, it may be the opposite.”
- “In some ways, it is more efficient and helps keep patients focused.”
- “It can be more demanding doing telehealth visits back-to-back all day.”
- “It takes time to adjust. But over time the provider, staff and patient become more comfortable.”
- “It’s a little more distracting and difficult to focus.”
- “Telehealth health visits are often more tiring, but the break from wearing a mask is helpful!”
- “Telehealth is exhausting in a way that office visits weren’t.”
- “The physical presence of a patient energizes me. This is a human being a few feet/inches away in need of care. With telephone or video, one loses that feeling.”
- “There’s less distraction and anxiety about a full waiting room when seeing patients remotely.”
- “There’s something about the technology that is more tiring. I have read that our brains are scanning for micro-expressions and other nuances that are available in face to face encounters, but that the technology is not advanced enough to provide us on video. Either way, it’s more exhausting, but I found that my stamina improved over time. There’s definitely an energy to being in the same room with a patient that is not present on video visits.”
- “They get very repetitive and difficult to sustain attention over time.”
- “This is less true if virtual visits interspersed with in-person visits, but then it’s harder to make schedule work.”
- “Virtual visits are very fast paced – I have to stay on point or I’ll fall behind.”
- “Weird that it makes such a difference to be with someone to feel relaxed and energized by the interaction, but it is true. When I have a full day of patients I know for televisits I do better. It is a huge strain to do effective care for new patients with no in-person component.”
- “When doing several telehealth visits in a row I find given myself a break in my schedule helpful.”
- “Works better than in office, can take a quick break between patients, grab a cup of coffee or a sweater or see a bird out the window (my office has NO windows) or pet the dog.”
- “Yes- great question! This is my biggest challenge. I do 100% video and the fatigue has increased compared to when I see people in person. I feel I have to work harder to “read” people and constantly staring at a computer strains my eyes. I miss face-to-face interactions significantly, it can also make the work feel much more isolating. It’s also difficult because natural breaks have been erased, patients are more often on time and it can sometimes feel like you are in a call center going from patient to patient.”
Please share any strategies or techniques you have used to prevent or reduce your fatigue in virtual visits:
- “Cutting back on patient schedule (doing less).”
- “Doing a mix of video and in person visits helps.”
- “I close the door, as if I was in an exam room, providing complete privacy, and turn off the outside world during the visit.”
- “I did noticed that blue light reducing glasses was helpful when I was working only video visits at the start of the pandemic.”
- “I don’t do telehealth visits back to back.”
- “I drink green tea! Try not to have more than two in a row. Make sure seat is adjusted properly.”
- “I encourage clients to minimize or shut down distractors (i.e., phones, ipads, other electronic screens) on their end during sessions when possible.”
- “I remember that the patient is counting on me to help them. I understand that they are getting charged just as much for a video visit as they are an in person visit and I do my best to give them my all.”
- “I take breaks and stand up and stretch every few visits. I am naturally someone who does not like to run around a lot so staying seated is not hard for me. I make sure to eat a protein filled lunch and breakfast so that I don’t have a carb crash afterward. I stand up at parts of the physical exam so that I can demonstrate how to do the exam to patients and serves as a refresh break. At the end of the day, I finish up and go for a very long several mile walk so that I can sleep well and be refreshed for the next day. Plus I do not use electronics at night.”
- “I write down things I want to address and start visit socially.”
- “If patients are walking around with their phone or computer, I’ve realized that gives me motion sickness and exhausts me, so I will be a little more proactive about coaching them on how to keep the camera still. I also get up and move around between visits. Also I try not to dive right into visits; having 3-5 minutes of social conversation really helps energize the encounter.”
- “I’m much stiffer with upper and lower back pain with virtual. If I have a phone visit (minority of visits) I stand and do stretches.”
- “It’s very difficult but I try to have a break every 3-4 patients (this can be near impossible at times). If someone no-shows I try to get out of the room and walk around my neighborhood to get my energy back up and reset my eyes.”
- “Much easier to focus on patients when you take out the element of checking in a patient and doing an exam. You’re actually better able to focus on the acute problem.”
- “My best medicine are my patients. Just being able to reconnect with them is a given. Making sure they are well. it is fun to see people you care.”
- “Need time for myself – usually take 30-45 minutes to exercise or do yoga between visits which helps with the fatigue.”
- “Schedule multiple modalities, diagnoses, and ages in a given day. Continue peer supervision weekly.”
- “Smile a lot – it brings out a smile in the patient and that energizes me.”
- “Snacks at my desk. I wish I would remember to get up between patients – I often get to the end of 4.5 hours of televists and find myself stiff, because I haven’t moved off my chair that whole time!”
- “Stand up between visits, schedule breaks, allow myself to get up and stretch even if it means running a little late.”
- “Stand up often. Move around, Get dance breaks. Between visits, hydrate! sing! Take a walk. Laugh!”
- “Standing desk is helpful.”
- “Try to find those pieces of the conversation that bring back the in-person feeling.”
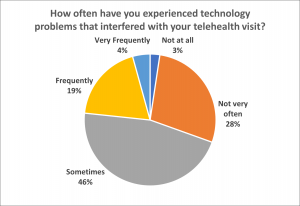
Comments:
- “Any issues were on the patient end for video calls. All telephone visits were fine.”
- “Occasionally phone drops call, but not commonly.”
- “Two or three times have had screen freeze with need to re-connect.”
- “Usually slow internet connection or patient’s issues with technology.”
- “Patients can’t get on video calls often. sometimes my remote access won’t work well.”
- “Power outages have been the biggest difficulty.”
- “Usually only happens in large groups meetings vs. 1:1 appts.”
- “A few power outages and a few bandwidth issues…less than 1% of sessions.”
- “Often there is a component on the patient side that doesn’t work well – freezing – or audio problems.”
- “Patient’s mobile device is too old for the video platform being used. Occasional glitches in the technology solution itself.”
- “I have patients who have difficulty using the video options. Occasionally the quality of the call became compromised and I had to call back and do straight telephone visit.”
- “Zoom freezes or connection is unstable. Occasionally sound does not work.”
- “Poor signal in afternoons. Problem usually on patient’s end. Difficult to hear patients sometimes when children or adolescents fail to talk in to the computer.”
- “Patient not technologically prepared.”
- “Typically has to do with Wifi strength and connectivity by the patient.”
- “It’s almost always on the patient side.”
- “Remote access dropping, patient cell service dropping, patients without unlimited data to allow for video visits, complexity of video visits (through google meet) prohibiting their use.”
- “Seems WIFI related on patient’s end, or video invites go to patient’s spam folder/can’t find it, which delays start.”
- “When working from home we get kicked off the server, sometimes losing notes and causing delay and frustration. Also sometimes the controlled substance prescription system doesn’t work, causing delay for important and sometimes weekly prescriptions. Also my computer screen is small, causing a lot of scrolling and searching for buttons. It has been frustrating to feel like we are on our own for technology at home.”
- “Calls have cut out during multiple visits, sometimes at sensitive times.”
- “Mostly unable to complete documentation in Epic.”
- “The patient might not have good service. Their voicemail might be full. If I need pictures sent through the patient portal sometimes patients have a hard time getting that up.”
- “Takes a long time to explain to some patients how to convert to a video visit, and sometimes we have not been successful.”
- “Families lack technology or can’t connect.”
- “My home office is the opposite end of the house from the WIFI and neither my home phone nor my flip phone worked reliably there.”
- “Patients are really struggling with the technology. The email option is cumbersome and delayed. Elderly patients really struggle.”
- “Typically related to connection/wifi strength.”
- “Usually issues with family ability to log in to the system. sometimes poor connection quality – audio or video or both.”
- “Audio is poor, frequent freezing.”
- “Getting disconnected from EPIC while at home.”
- “There is such a wide range of devices that it’s hard to help sometimes when things go wrong.”
- “Slow internet access causing frequent shut down of our EHR. Poor phone connection with patients.”
- “If a client is using a phone and they get an incoming call the audio drops on videocall.”
- “Slow EHR, poor quality video, interpreter drops off session. Much eye strain doing video sessions on a 13″ laptop screen.”
- “Training elders several times before success, interruptions or disconnected when client gets a text or phonecall, wasted time sending out links weekly to clients that aren’t able to access from a previous link.”
- “Video glitches are fine but audio issues are so annoying as I am worried about missing important things my clients might be saying.”
- “Too many to describe.”
- “Getting kicked off Epic, disconnected from telephone interpreters; the instructions for video visits never worked for me.”
- “On patient’s end.”
Please share any strategies you have been using to effectively address technological issues in virtual care:
- “Being able to use multiple modalities is helpful, but our institution has limited this (for example some patients can handle Facetime but not Google Meets, but even with their permission per our employer we are not allowed to use this).”
- “Call back to see if connection improves.”
- “Doing telephone only. Video is almost impossible.”
- “Don’t waste time; go to another modality ASAP.”
- “Enlisting help of staff in facilities, family members ahead of time who are using more digital communications themselves.”
- “Go to a clinic with a wired computer.”
- “Have resource staff who are tech savvy available to help.”
- “Have the Medical Assistant work with the patient 10-15 minutes before the visit to make sure they are able to login to the virtual waiting room.”
- “I bought a large screen so I could see everything at once. This was revolutionary. I moved my work space closer to our server, that helped internet speed some too. We bought the most expensive home internet service as well. Our group has a whatsapp thread and we often problem solve together.”
- “Instructions are emailed to the patient 24 hours prior to the visit so any issues can be corrected before the visit.”
- “Learn how to trouble shoot for various devices, especially mobile devices. Understand workarounds when integrated solution does not work (e.g., ability to send email or SMS invite).”
- “Making sure I pay for improved WIFI speeds at home.”
- “Medical Assistants do virtual rooming, call patient in advance and ensure they are adequately set up for connection.”
- “Our office has one dedicated staff member who is available to reach out and troubleshoot with patients on short notice (or ahead of time, if family expresses concerns about their ability to figure out the service).”
- “Prayers. Also disconnected other devices from internet – e.g. cell phone, Ipad. Bribing kids to get off internet.”
- “Proactive outreach by technical support to first time users.”
- “Re-configuring home internet setup. Using earphones/headsets for best call quality.”
- “Routers in every room.”
- “Setting up a plan in advance with patients in case of technological issues (e.g., if internet fails, I’ll call you; if sound is delayed, try turning video off for a moment, etc.)”
- “Sometimes it is as simple as logging in and out again. Other times, I use the audio on my phone and the video on my computer, and that seems to resolve the issues. I also close out other apps or webpages on my computer, which tends to interfere with connectivity.”
- “Try and get patients to situate themselves closer to their router if possible.”
- “Use telephone only – video is too hard.”
- “Using the “join phone audio” option through the Zoom app once I’m signed in. Even if the video freezes briefly, I don’t lose audio with the client.”
- “We are trying to support each other in the practice. Staff are trying to get patients set up, but the time needed to do so is difficult.”
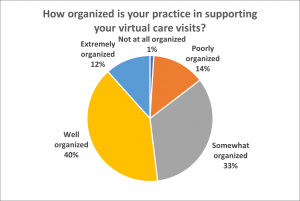
Comments:
- “A pre-communication about how to engage in a video visit would be great.”
- “All clinicians have jetpacks and chromebooks and there is an IT department that can be reached for support.”
- “All the teaching about telehealth and troubleshooting is being done by providers. It would make more sense to have a dedicated team for this.”
- “Differences between how psychiatry does televisits (which we pioneered in our system during COVID) as opposed to primary care (which has been slower to adopt but has more sway in determining workflows).”
- “Difficult to coordinate front desk staff and medical assistants with televisits because all in different locations. Checking out patients isn’t the same process where they can have their follow ups booked and specialty appointment referrals reviewed.”
- “EPIC and Google Meet are now combined which is great.”
- “For clinicians that work in low income areas, doing a video visit presents challenges on multiple levels. I don’t feel my organization has taken this challenge very seriously and is still trying to have patients do a Google Meets video visit. Many people do not have a smart phone service that can support this and many, many patients can’t get the technology to work.”
- “Good training and support.”
- “I am not aware that anyone is working on this, maybe they are….”
- “I could use a lot more technical assistance in getting patients set up for video visits.”
- “I just tell the staff to give my encrypted email and have the patients email me directly to schedule their virtual visits.”
- “In person appointments are stressed, and we no longer have dedicated blocks of time for virtual visits.”
- “It does not seem that it is well embraced by some of the senior providers and there is a lukewarm acceptance from middle management. For instance a lot of the clerical part (entering the patients email, placing the patient in the virtual wait room) are left to the providers to handle.”
- “It is possible to conduct virtual visits on site if needed, but there is not technology support for home internet issues.”
- “It takes A LOT of resource to get patients up and running and our teams are strapped with increased volume demands, staff shortages, and depleted resilience with the pandemic.”
- “Mostly due to short staffing due to pandemic redeployments.”
- “Need virtual rooming by MAs and calls beforehand to prep patient, get vitals, review meds, update immunizations.”
- “No clinic-based structure to support video visits.”
- “On call technical support available to outreach to patients/families.”
- “Organization is starting to listen to us as far as simplifying things.”
- “Our clinic is outstanding at supporting these visit and clearly finds it to be critical to the mission to provide safe and effective health access.”
- “Our IT staff is great, but has been a huge burden.”
- “Telephone visits are well organized, but video visits are still poorly organized.”
- “Telephone visits have basic organization –televideo, however, is very, very rudimentary, and basically has the feel of ‘provider on their own’ if there are challenges with access to video, tech challenges, patient tech literacy.”
- “The hospital is still adapting.”
- “The original plan was for patients to be called 15 minutes prior to telehealth to be checked in. This rarely happens due to how busy they are at the front desk. I usually just have the front desk check them in after my visit so I can document.”
- “The RN/MA calls and “rooms” the patient.”
- “The staff are unable to help out with using zoom due to time constraints. Though I am very adept at using zoom, I am not using it to see patients via telehealth because there is simply no time for me to call patients, set them up on zoom, email them, etc. with links.”
- “We have a terrific Clinical Applications team and a terrific IT team, and our administration has done a good job in this area.”
- “We have an IT remote tech team who is available as needed throughout the work week.”
- “Well organized for phone visits. Not at all organized to assist patients with video.”
Please share any strategies you have used to involve the other members of your care team in your telehealth visits:
- “Conferencing them in on patient telehealth visits.”
- “Front desk staff will send out email invitations for patients to connect for the telehealth visit after confirming proper email addresses. Coding/billing team has been involved from the start to ensure that is done properly given the frequent changes by insurers and visits are billed for.”
- “Front office staff make contacts with patients, via telephone and does COVID-19 screening (esp. needed prior to home visits now w FLU Vaccines being administered in home). Staff will screen and schedule appointments (while I focus on case management, pharmacy calls, follow-up on labs tests, medications use in home, med delivery services, social issues such as setting up Hospice, MOW, HHA, home makers).”
- “Having them observe video visits with permission from family.”
- “I am in the process of developing a Virtual/In Clinic team with front desk, nursing and support staff representation with specific tasks and work arounds to make the encounters proceed more smoothly. I also hope to include a patient representative in this team building effort.”
- “I forward follow-up plans to the front desk, letter writing, phone calls, to MA’s, etc. queries that nursing needs to make consultations to other providers. I find doing them within that visit optimal vs. saving for the end of the day, whereas there would be too many issues to deal with.”
- “I have no contact with my team.”
- “I set things up for myself.”
- “I set up 2 computers (or split screen) to allow for talking and documenting at the same time. My staff reviews demographics and insurance information as well as a quick HPI before I come to the computer (frequently the night before). My staff calls the patient a few minutes before the start of the appointment to let the patient know when to go to the waiting room. My secretary and MA are both trained to set up and log into the platform I use. When I sit down, I am (usually) ready to go.”
- “I think the benefit of telemedicine is that the provider can talk directly to the patient without a bunch of bulky screeners, forms, etc etc etc. This is the administrative bloat of medicine. Trying to “incorporate other team members” for the sake thereof is pointless. (For reference I am a young provider, strongly believe in team-based care, but not just for its own sake.)”
- “MAs call ahead, “room” patients, work on getting them on the video call ahead of time.”
- “Review in team meetings; sharing learnings with each other.”
- “Secretary confirms appointment and that program is running properly.”
- “Teaching the medical secretaries and triage nurses the different telehealth formats.”
- “Team members are scheduled to assist providers. They call patients in advance to complete forms. They try to help patients sign up for MyChart and send photos. Sometimes this is successful and sometimes it is not.”
- “They are well trained and see it as part of the mission and act speedily and effectively to support our patients–and support one another–to ensure telehealth meets the highest standard and is a success.”
- “They do intake and make sure the patient knows how to log in. Sometimes going through steps with them and virtually “rooming them.”
- “Try to keep workflow as consistent as possible between in-person and virtual visits. Front desk staff does pre-check in ahead of time, MA’s do rooming tasks, etc.”
- “Virtual ‘huddles’ with medical assistants who virtually ‘room’ patients to get them ready for visits.”
- “We are all on at the same time when needed.”
- “We are not doing much to support clinicians at this time, need virtual rooming and post-visit workflows to be improved.”
- “We have front desk staff booking patients into our schedule. There’s a good flow of communication between providers and front desk to book follow ups. I have been mostly doing phone calls, and have not encountered any major issues.”
- “When using interpreter, call the interpreter first on the virtual visit, then have the patient join.”
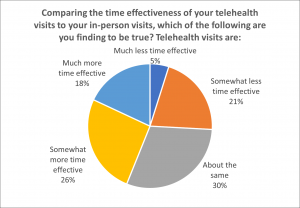
Comments:
- “A lot of the after-visit scut work falls on the provider.”
- “After getting the initial tech issues out of the way and orienting patients to the different procedural and boundaries in telehealth, it is very effective with fewer missed visits.”
- “At times setting up the initial telehealth visits is a longer process. But once set up, patients, families and staff find it very quick and easy.”
- “Clients are more committed to appointments and easier to schedule and meet with.”
- “Cons: We have to spend session time on technology issues. Pros: More clients showing up to virtual visits.”
- “Families never seem to have weights or temps taken ahead of time as requested. Always seem to be delays with connections.”
- “Fewer no shows so can’t use that time for paperwork. More difficult to end session. Time spent trouble shooting. Calling back when people don’t answer the first time.”
- “For the patients, a 30 minute visit takes 30 minutes. An in-person visit for the patient it is more like 3 to 4 hours if you count travel time, parking time, signing in, and waiting for late staff or doctors.”
- “Hard to do with people who don’t hear well, and need phone interpreter.”
- “I can complete documentation during the visit. It is easier to limit the time during the visit.”
- “I can type while talking without offending the patient.”
- “I spend more time directly with patients and they avoid waiting in our waiting room or in transit.”
- “I spend more time taking to patients.”
- “I use the whole 45 minutes as therapy time because there is no check-in at the front desk or commute time/traffic that might make the client a couple minutes late (assuming no technical issues).”
- “It depends on the patient and the situation. Some visits take longer, others take less time.”
- “It feels like it takes double the time to accomplish half as much. Patients and providers are not used to this type of interaction and often patients aren’t ready for the appointment. It’s easy to interrupt each other and harder to have a natural conversation without seeing each other. Language barriers are amplified as we can no longer see non-verbal cues. It takes time to get the interpreter on the phone. I have not successfully completed a video visit call as there are too many barriers for my patients. They are unable to set up the call or use the right app to make the video work. They also don’t have the time and may be too busy to set this up. We usually just do regular telephone because of this.”
- “It is challenging to complete some of the work as there is much distraction on the client’s side.”
- “It’s harder to keep the conversation going through telehealth.”
- “It’s much more difficult to end a session via telehealth, most clients are isolated and I’m the only person they see or talk to.”
- “Less commute for patients and time doing vitals and walking from place to place.”
- “less travel time; but greater initial time wasted teaching patients how to access/use the technology.”
- “More time effective, but not as clinically effective.”
- “More time-effective only in that I’m working at home so there’s no commute. Other than that, it’s the same.”
- “No ability to gauge nuances.”
- “On average, about the same. For known patients, it’s less time, for new patients to the clinician it’s more time. Within a clinic session it’s about the same overall time.”
- “One loses out on the vital signs and clinical exam, and so can be considered less effective if I have to invite the patient to be seen again, in person, to address the same issue.”
- “Seeing a lot more clients because I don’t have to allow for them to travel to the office. Also if I get a no show it is much easier to meet with another client simply by calling them as opposed to having them be able to travel to the office.”
- “Some visits are longer and somewhat more complicated (for example if interpretor needed or if drawing a picture would help clarify for patient), but other visits are far more time efficient. On balance it is likely about the same.”
- “Some visits take less time and some take more time from an efficiency standpoint. May save on rooming/processing time if it is straightforward, but lose on time when other aspects need to be done (e.g., screening forms, arranging tests, follow up visit for issue which can’t be addressed virtually etc.).”
- “Sometimes it is the same, but sometimes getting the technology to work is a hurdle.”
- “Sometimes saves time.”
- “Take significant time when interpreter is needed.”
- “Takes people time to get technology set up.”
- “The follow up work is done by the provider which adds extra time (f/u visit, #’s for consults).”
- “The time saved by absence of a physical assessment is gobbled up by increased time setting up labs and follow up appointments, and also dealing with technology.”
- “The visit itself is more time effective, but given technology issues and barriers, they overall become less time effective.”
- “The visits don’t usually last as long as in-person, but since I type my notes instead of handwriting them, documentation takes three times as long.”
- “There are much fewer no shows.”
- “They take less time, but also accomplish less. Physical exam cannot be done via telephone!”
- “Time efficacy is hindered by the number of times a follow up visit is needed for an exam. Preparation for mental health visits (e.g. sending out standardized questionnaires and getting them returned and scored) is more inconsistent and difficult with telehealth (though number of ‘no-show’ visits for behavioral health seems to be less).”
- “Time saved with rooming/delays in arriving/parking etc., but more time if needing to assess something that in person may be easy to ‘look at’ like an ear, rash, etc.”
- “Transit time is omitted and no shows are much less likely.”
- “When it works well, virtual can be more time effective.”
- “You’re scheduling clients back-to-back with no wait time and fewer missed appointments.”
Please share any strategies you have used to improve the time effectiveness of your virtual visits:
- “Allow for in person visits when needed and don’t try to use the virtual for topics not ideal for it.”
- “Clinicians need to be organized and it has cut down on the number of missed appointments.”
- “Deal with one issue and have patient follow up in short interval to deal with others.”
- “Discipline. Treat the visit the same as an in-person visit.”
- “Document at the time of the visit while I am talking to the patient (I let the patient know ahead that I have her record on another screen ahead of time so she doesn’t think I am checking my email). Send in prescriptions and order labs before you end the call.”
- “Document notes in real time. Deploy students (if patient consents–and so far 100% have). Call patients before procedures for review informed consent or questions.”
- “Front load my schedule heavy on Monday and Tuesday and if I get a cancel or no show it is a lot easier to see them later in the week as opposed to if my no shows happened on Thursday or Friday.”
- “Get pictures for derm questions.”
- “Have sent clients information and supporting literature by email or have printed such materials and mailed them.”
- “I follow a template.”
- “I have informed clients that the timer starts from when the link is sent and not when they decide to log on.”
- “I have the patient video on one device and then I can notate on my main laptop so that the time spent with them is productive and face to face at the same time.”
- “I type my encounter notes during the televisit which allows me to be more efficient and save time. Whereas in clinic, I like to show the patient that they have my full attention, so typing is minimal.”
- “I use my phone for the video/voice to free up the computer screen for typing/reviewing data.”
- “I will send text and then call patient to let them know that I sent them a text. The link is in the text body and they just have to click the link.”
- “It is easier to set limits on a call vs. face-to-face, and also I feel less guilty setting limits as I know the patient has not taken off time for work and travelled and is paying for parking to reschedule to complete.”
- “Keeping track of which patients won’t answer blocked numbers or will only answer second call. Sending email requests for televisits twice in case first one does not get through. Booking certain patients for longer times since are consistently taking longer to get started.”
- “Precharting, sometimes informing patients that there is a patient waiting so the visit will be ending soon.”
- “Pre-populating note with past history, and previous concerns related to visit topic.”
- “Set up laptop adjacent to another computer so documentation in the EMR is happening concurrently.”
- “Sharing my screen to help the client see scales in order for it to be more time effective.”
- “Targeting triage so that televisits are not used for certain conditions (vaginitis, ear pain, etc).”
- “The biggest issue is assisting people in understanding they cannot be doing other things in session, can’t be driving their car, need to be alone for the session, etc.”
- “When home, scanning and sending information to patient or office takes more steps.”
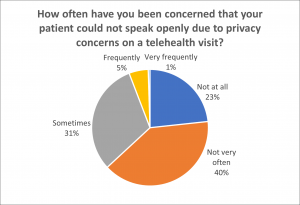
Comments:
- “Always needs to be addressed when dealing with adolescents and mental health. (‘the walls have ears…’)”
- “But, I could be fooled because I usually don’t do video visits.”
- “Depending on their location with the need for internet and who is in the house or area, especially if they are homeless or need to go somewhere to get internet.”
- “Helicopter parents can be an issue.”
- “I always assess that the patient is a safe and private location before proceeding.”
- “I ask and re-ask at the outset and then within the visit and all patients for all visits so far have expressed they were safe and able to speak openly. AND, this is with a cohort of patients that have more trauma than the general population. I take this seriously and know that (a) I could be missing something and (b) trauma is ubiquitous so this may underrepresent the reality, but so far I have sought but not received any patient concerns.”
- “I can often hear others in the background during telehealth visits and worry about privacy.”
- “I have very few concerns. When I do, I request that they move to a more private location in order to maintain privacy and focus on therapy session.”
- “Important issue I address at the beginning with all adolescent telehealth visits.”
- “Making sure teens can speak privately can be an issue, though usually they are able to go to a bedroom and shut a door.”
- “None of my clients have experienced problems with privacy.”
- “Often patients are home with family and don’t have a private space or get interrupted by children during sessions.”
- “Only occurs with more acute patients who have serious mental illness/psychosis/paranoia.”
- “Other household members in the background.”
- “Patients are often not in private settings especially those who have to work. Often patients are calling from work. Also, I have concerns about patient’s calling in the presence of others/family members and not being able to speak freely especially about things like abuse.”
- “Patients call from bathrooms, cars, outside to ensure privacy.”
- “Patients frequently answer calls in public.”
- “Patients have been worried about talking when people were at their homes.”
- “Patients sometimes have to take calls sitting in their parked car or in their bathroom because there is no other private space in the house.”
- “People living in close quarters often do not have private areas to talk.”
- “Probably about 5% of calls.”
- “Smaller siblings don’t understand boundaries or students will be with friends at time of the appointment.”
- “Some clients are in an abusive relationship and have to hide the call from their partners. Parents of children doing remote learning have a hard time focusing or have to schedule for later afternoon.”
- “Sometimes patients forget about their appointment so they are at work or in public.”
- “Specifically patients with history of Intimate Partner Violence or with teens.”
- “This is a big problem with adolescents.”
- “This is a major concern for my adolescent patients. It is never clear how alone they are.”
- “This is one of my largest concerns with telehealth. I have had numerous occasions during which confidential therapy appointments have needed to be interrupted because the patient was out in the community when they indicated they were at home.”
- “This is particularly true with child clients who are set up in the living room with other family nearby.”
Please share any strategies you have used to ensure your patients have a private and/or safe environment for your telehealth encounters:
- “Address early in session, problem-solve lack of privacy at either end.”
- “Ask the adolescent if they have a private place to speak away from everyone else before starting the visit. Be aware of who is in the background who can’t be seen on the video.”
- “Ask the patient to see if they can do the visit and feel they have sufficient privacy– which is not effective if the patient is in the same room with a violent partner or someone else who may inhibit patient from expressing what is truly going on.”
- “Asking the client either through the audio or a chat feature to make sure they are safe.”
- “Asking yes/no questions can be helpful if they are on the phone in a more shared space but have headphones in, etc.”
- “Code words for whether they are able to speak, adjusting meeting times, etc.”
- “Encourage use of headphones, typing in the chat when needed.”
- “I ask if it is okay to talk. I will reschedule if it is not a good time. I will ask yes/no questions. If I have the sense something is not right I will try to make an in person visit.”
- “I have encouraged clients and staff to close their doors while on telehealth, use headphones, noise machines, noise machine phone appointments, or air purifiers to block out sound.”
- “I have not done this, but other providers have told me they ask teens to spin around and show them the room they are in to ensure it is a private conversation.”
- “If I suspect that a teen, in particular , is not in a position to speak privately, I encourage them to take the phone into their room, bathroom or even outside to the car! It’s usually not a problem. Most of my parents relish the opportunity for me to speak privately with their teens.”
- “If they do not have privacy, part of our discussion is to strategize on how to make that happen at our next visit.”
- “Invite teenage clients to use headphones or microphone.”
- “Send email beforehand with telehealth visit suggestions to protect privacy, etc.”
- “Set patient expectations about where they should be at the time of the visit/call.”
- “Sometimes patients will sit outside in their parked car if they need a private space to talk and don’t have a room in their home.”
- “Start every session by inquiring if client is in a confidential spot to start session. Ask them directly if they have any concerns about speaking freely. If client has access, try to have them do session through HIPAA compliant platform Zoom.”
- “Very strict guidelines and expectations about others having people around, also use private chat feature when needed.”
- “When I suspect there is some layer of reticence or lack of clarity, I ask “can you freely speak to me where you are?” People tell you.”
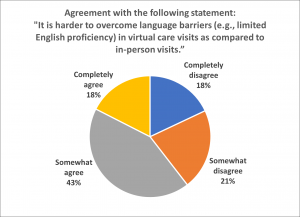
Comments:
- “A poor phone connection can make even a visit in English difficult.”
- “Always more difficult with phone interpreter than face-to-face.”
- “As a visual person, a mask is more difficult for me to overcome language issues than the video.”
- “Being hard-of-hearing myself as an older clinician, even with hearing aids, it is hard to understand some accents. Speech is harder without seeing faces.”
- “Connection quality is often poorer when using an interpreter.”
- “Difficult to use interpreters.”
- “Easy to get interpreter.”
- “Either way I use the telephone interpreter. It can be hard to not have body language on the phone.”
- “Gestures and body language are not as clear.”
- “Harder at times to understand, especially when it is a phone visit.”
- “Has been easier to get phone interpreters than in-person interpreters.”
- “I can always count on the family network.”
- “I don’t know how one would arrange for translation on a telehealth visit.”
- “I don’t run into this issue much, but when there is a language/cultural barrier, it is more effective in person.”
- “I usually ask if a family member can translate to be sure no adverse events or side effects from medications.”
- “If you’re having trouble hearing consistently, it makes it harder.”
- “Interpreter services have worked equivalently on our platform (can still be slow to activate, but once linked, there is no difference in the pace of the conversation).”
- “It depends on whether the session requires review of documents, but the biggest issue is whether the interpreter is proficient and comfortable with the medium.”
- “It has shown to have about the same amount of challenges.”
- “It is not always challenging, but very frequently in-person visits would be much more helpful for body-language and other subtle things that are lost in translation.”
- “It is not harder to overcome in my experience, but to ensure this is not a barrier, it is somewhat more time consuming.”
- “It’s awkward and I typically use my landline to call the interpreter while I use doximity for the patient videocall. Zoom would be a better platform, but that is dependent on having staff available to set this up.”
- “Lag in internet causes more confusion, as does face-to-face outdoor visits with masks.”
- “More reliance on family members to help with translation. Language line would have to be via telephone, which is not preferred over video.”
- “Not having non-verbal cues makes it incredibly difficult. Interpreters lengthen the time of visit. We can’t review medication vials or blood sugar readings and rely on the patient to read them to us.”
- “Our patients don’t have access to stable wifi/data allowances to permit video visits, so losing non-verbal cues also makes communication difficult when the patient has limited English proficiency or the phone interpreter is having difficulty.”
- “Same difficulties over phone vs. in person.”
- “Sometimes the sound is garbled or there is a delay and the video is hard to read (body language).”
- “Translation is always on audio/telephone even when patients are seeing me in person.”
- “Translation services are never hard to reach. It just makes the encounter twice as long.”
- “Use of interpreters can be more time consuming since they are not on site. With phone visits don’t have advantage of being able to see the patient’s expressions which can complement the interpretation.”
- “We often used phone interpreters in face-to-face visits anyway, so it feels similar now.”
- “We use interpreters on the phone in clinic and now on the phone in virtual, so the interface is exactly the same.”
- “We use telephone interpreters either way, so it feels about the same.”
Please share any strategies you have used to overcome language barriers with your patients in telehealth visits:
- “3 way calls usually work.”
- “Adjusting volume on cell or speakers helps, asking to repeat always helps.”
- “Ask if interpreter can do video; have interpreter join the call before the patient.”
- “Continue to check for mutual understanding.”
- “Have a family member present.”
- “Have also used I-translate from Iphone if client stuck on a word or two.”
- “Have interpreter in the room with me, but that has its own issues in terms of social distancing.”
- “Having a bilingual second staff.”
- “High volume, take our time.”
- “Hire more bilingual staff.”
- “If the history was too difficult to obtain over the phone, schedule the patient for an in person visit.”
- “Keep answers short.”
- “Offering interpreter services from the start. My scribe contacts patient and determines language needs before we merge our calls for the encounter.”
- “Reaching out to ICC & DCF if they are involved and can provide translating.”
- “Schedule a little more time and call the interpreters before to give some briefing and make plan together.”
- “To be prepared to run late because the visit simply takes more time.”
- “Typing when necessary.”
